Key Takeaways
- Tooth decay develops in stages:
- What causes decay?
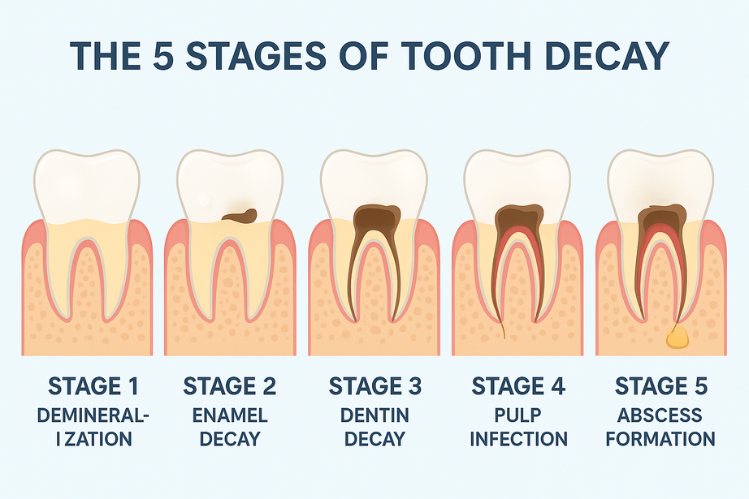
- The 5 stages of tooth decay:
- Prevention is always better:
- Sealants and fluoride treatments:
- Clear aligners:
- Bottom line:
It doesn’t happen overnight. Catching it early makes treatment easier, less painful, and often less costly.
Plaque buildup from poor oral hygiene and sugary foods breaks down enamel, leading to cavities, infections, and even systemic health risks if untreated.
Demineralization (Pre-Cavity): White spots; reversible with fluoride.
Enamel Decay: Visible dark spots or small holes; requires fillings.
Dentin Decay: Sensitivity to hot/cold; fillings or crowns needed.
Pulp Infection: Severe toothache; treated with root canal and crown.
Abscess Formation: Extreme pain, swelling, fever; emergency treatment, sometimes extraction.
Brush twice daily with fluoride toothpaste, limit sugar, drink fluoridated water, avoid frequent snacking, and see your dentist regularly.
Provide extra protection against cavities, especially for children and high-risk patients.
Help prevent decay because they’re removable, easier to clean around, and don’t trap food like traditional braces.
Tooth decay is preventable and treatable at every stage, but early action is key to saving your smile and avoiding serious health risks.
Tooth decay, one of the most common dental problems everywhere, but it does not appear suddenly, not overnight. Cavities, they sort of arrive in steps, starting small, changes you may barely notice, then slowly, if left alone, moving into painful infections that risk not just your teeth but overall health too. The upside? Every stage has some kind of treatment, and the earlier it’s spotted, the easier, often less costly, to manage or fix.
In this guide, we’re going through five stages, what each looks like, how it feels, and the treatments that, really, can save your smile.
What Is Tooth Decay?
Tooth decay is the gradual breakdown and rotting of the tooth structure because of acid buildup and plaque. This can happen due to overconsumption of sugary foods and poor hygiene.
When you don’t brush your teeth properly after consuming sugary foods and drinks, it creates plaque around your teeth, which in turn turns into hard tartar. This acid-producing environment weakens your enamel, eventually causing cavities, infections, and even tooth loss.
Why does it matter? You know, untreated decay doesn’t just mean rotting teeth. In advanced stages, the bacteria can spread into your bloodstream. This is leading to systemic infections that affect your entire body.
This is why understanding different stages of tooth cavity and decay can help you find the issue early on.

The 5 Stages of Tooth Decay
Here’s a breakdown of the 5 stages of tooth decay:
Stage 1: Demineralization (Pre-Cavity Stage)
- What happens: Plaque acids begin dissolving minerals from enamel. The tough outer layer. This is the stage 1 early cavity, also called the pre-cavity stage.
- Signs: You might notice white chalky spots or faint lines. No pain, not dramatic, but the beginning is there.
- Reversibility: At this stage, it’s often reversible; fluoride toothpaste, professional fluoride treatments, and diet changes can help rebuild enamel.
Learn more about the effects of tooth decay and why spotting early stage brown tooth decay or white spots matters.
Stage 2: Enamel Decay
- What happens: The enamel breaks down further. Cavities form, visible on the surface. This is one of the most noticeable stages of cavities.
- Signs: Brown or dark spots, pits, or even small holes. Sometimes food gets stuck.
- Treatment: Once enamel is gone, it cannot grow back. The usual tooth decay medical procedure here is a filling, or a crown if the damage is more severe.
Most patients only realize at this point, too late for reversal, and professional care becomes essential.
Stage 3: Dentin Decay
- What happens: Bacteria move into dentin, which is softer than enamel. Decay speeds up.
- Signs: Sensitivity to hot, cold, and sweet foods. Sometimes, there is a dull ache.
- Treatment: Fillings or crowns are used depending on the damage. If ignored, it quickly advances to pulp infection.
This is not just a “cavity” anymore; it’s a deeper stage, more serious, and much harder to ignore.
Stage 4: Pulp Infection
- What happens: Decay reaches the pulp, the inner chamber with nerves and blood vessels.
- Signs: Severe toothaches, gum swelling, throbbing pain that won’t let you sleep.
- Treatment: A root canal—the standard tooth decay medical procedure here—removes infected tissue, disinfects, and seals the tooth. Often followed by a crown.
Skip this treatment, and the problem escalates into a dangerous abscess.
Stage 5: Abscess Formation
- What happens: The infection spreads beyond the tooth to the root tip and bone, forming a pus pocket (abscess).
- Signs: Extreme pain, swelling in the face or jaw, fever, swollen lymph nodes. Sometimes pus drains through the gum.
- Treatment: This is an emergency. Dentists may drain the abscess, prescribe antibiotics, and attempt a root canal. If the tooth can’t be saved, extraction is the only solution.
At this final stage, it’s more than oral health; it’s a risk to your entire system.
Why Prevention Is the Best Cure
Stopping tooth decay is always easier than fixing it later. A few simple daily habits and regular checkups can make the difference between a healthy smile and dealing with painful dental cavities or even rotting teeth. The good news? You can often catch problems like a stage 1 early cavity, pre-cavity enamel damage, or those faint early stage brown tooth decay spots before they turn into something serious. This is what you can actually do to reduce the risk of tooth decay .
- See your dentist regularly
- Brush your teeth twice a day
- Limit sugary foods and drinks
- Drink tap water when you can
- Avoid frequent snacking
- Ask about dental sealants
Routine checkups and professional cleanings help catch the early stages of cavities before they become serious. Dentists can also recommend treatments like fluoride or sealants as part of a tooth decay medical procedure to protect your teeth.
Use fluoride toothpaste and brush after meals whenever possible. This strengthens enamel and reduces the chances of plaque leading to pre-cavity spots.
Candy, cookies, and sodas feed the bacteria that cause decay. Cutting back on sugar helps prevent both early cavity signs and advanced tooth damage.
Most tap water contains fluoride, which naturally strengthens enamel and helps fight decay.
Constant snacking gives bacteria more sugar to turn into acid, speeding up the stages of cavities. Stick to balanced meals instead.
Sealants are thin protective coatings placed on the chewing surfaces of your back teeth (molars). They block food particles from getting stuck in deep grooves, lowering your risk of early tooth decay.
How Clear Aligners Play a Role in Decay Prevention
If you have misaligned teeth, this can be a reason for plaque buildup. This means you need to straighten your teeth to ensure better cleaning between teeth. Now you need to know that not all teeth straightening methods are the same. While braces can trap food, which leads to plaque. Clear aligners, on the other hand, are:
- Removable: You can brush and floss normally, keeping your teeth cleaner.
- Smooth-surfaced: They don’t provide hiding spots for food debris.
- Health-friendly: By lowering plaque buildup, they also reduce the likelihood of early-stage brown tooth decay.
If you’re considering orthodontic treatment but want to minimize decay risk, clear aligners are a smarter, more hygienic option.
Finally, Can I Stop Tooth Decay?
Tooth decay doesn’t happen all at once. It progresses through five distinct stages, from early pre-cavity signs like white spots to dangerous abscesses that threaten your health.
The earlier you act, the easier (and more affordable) treatment is. Don’t wait for pain to tell you something’s wrong. Schedule preventive care today and protect your smile for the future.
FAQs
1. Can early tooth decay heal on its own?
In some cases, especially the early stage of tooth decay, you can reverse the symptoms by using fluoride toothpaste, following good oral hygiene, and eating non-sugary healthy foods.
2. How do I know if I need a filling or a root canal?
It all depends on your symptoms. For a surface issue that only affects your dentin and enamel, then filling will be enough. But if the pain is sharp and constant, then that likely means that your pulp has been affected. This will need a root canal.
3. Is tooth sensitivity always a sign of decay?
Not always. Sensitivity can come from worn enamel, gum recession, or even whitening products. But persistent sensitivity should be checked by a dentist.
4. Can clear aligners reduce the risk of cavities?
Yes. Since they’re removable, clear aligners make brushing and flossing easier, lowering the risk of plaque buildup compared to traditional braces.
Citations:
Information, National Center for Biotechnology, et al. Tooth Decay: Overview. Www.ncbi.nlm.nih.gov, Institute for Quality and Efficiency in Health Care (IQWiG), 27 Feb. 2020, www.ncbi.nlm.nih.gov/books/NBK279514/.
Cleveland Clinic. “Cavity & Tooth Decay: Causes, & Treatment | Cleveland Clinic.” Cleveland Clinic, 27 Mar. 2023, my.clevelandclinic.org/health/diseases/10946-cavities.