Key Takeaways
- Definition:
- Prevalence:
- Causes:
-
Symptoms:
Mild: Slight misalignment, minimal discomfort.
Moderate: Difficulty chewing, speech problems, jaw pain.
Severe: Visible jaw protrusion, TMJ disorders, and breathing issues.
- Diagnosis:
-
Treatment Options:
Orthodontic: Braces, clear aligners, expanders, reverse-pull headgear.
Surgical: Orthognathic surgery, bone grafts, or implants for severe skeletal cases.
Early Intervention: Growth modification devices in children can prevent worsening.
- Complications if Untreated:
- Prevention & Detection:
- Living with an Underbite:
- Prognosis:
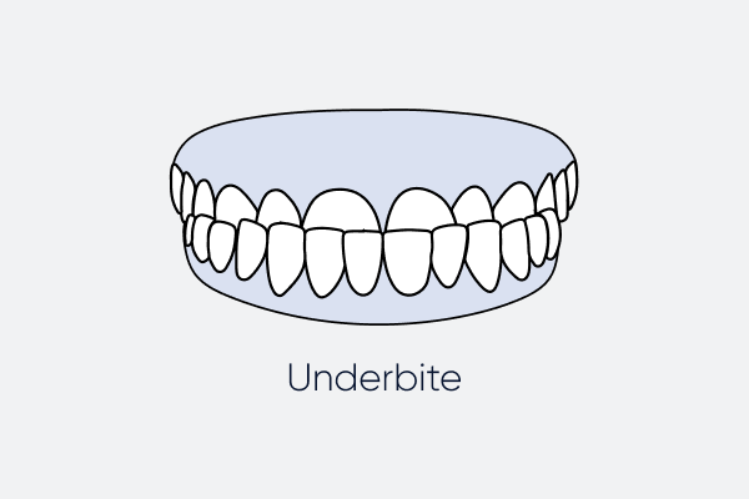
An underbite, or Class III malocclusion, happens when the lower teeth extend beyond the upper teeth, affecting bite, function, and appearance.
Around 5–10% of people experience some degree of underbite, ranging from mild to severe.
Common causes include genetics, childhood habits (thumb-sucking, tongue-thrusting), jaw trauma, congenital conditions, and, rarely, jaw tumors or growths.
Dentists use physical exams, X-rays, cephalometric analysis, and 3D imaging to determine severity and treatment needs.
Can lead to tooth wear, gum disease, TMJ pain, difficulty chewing, speech problems, sleep apnea, and reduced self-esteem.
Early dental checkups (by age 7) and addressing harmful habits can help reduce severity.
Requires good oral hygiene, dietary adjustments, and emotional support during treatment.
With timely intervention, an underbite is highly treatable, restoring both function and confidence.
Generally, a smile tends to be one of the first characteristics that a person notices about you, as it helps your appearance while also making a great first impression on others. Malocclusions are now seen in individuals of all ages. An underbite is a type of malocclusion, along with an Open Bite , overbite, Crossbite , or crooked teeth that many experience. An underbite occurs when your lower teeth extend past your upper teeth while you bite. In this blog, let’s find out everything you need to know about an underbite: its causes, types, and how to correct underbite.
What is an Underbite?
An underbite, clinically referred to as Class III malocclusion, is a dental condition where the bottom front teeth overlap or project past the top front teeth. Unlike a slight misalignment, an underbite can impact not only appearance but also jaw function. Detecting it early is crucial, since untreated cases may result in jaw pain, speech problems, tooth damage, gum issues, or even breathing difficulties.
Types of Underbite
Before you ask, can an underbite be fixed? You need to know that not every underbite is the same. Knowing the type helps decide the right treatment plan.
Dental Underbite
- Happens due to tooth position, not jawbone structure.
- Occurs when teeth erupt at the wrong angle or crowding pushes them forward.
- Easier to fix with orthodontic devices such as braces or aligners.
Skeletal Underbite
- Caused by jawbone irregularities, often inherited.
- The bottom jaw grows too far forward, or the top jaw grows too far back.
- Usually requires orthodontics combined with jaw surgery.
Functional Underbite
- Forms due to habits in childhood or temporary growth issues.
- Typical triggers include thumb-sucking, tongue-thrusting, or long-term pacifier use.
- Early treatment in children can often reverse or reduce this form.
Symptoms of an Underbite
Symptoms vary depending on the severity of misalignment.
Mild Symptoms
- Slight upper and lower tooth misalignment.
- Little to no discomfort.
- May not notice issues unless chewing tough foods.
Moderate Symptoms
- Chewing problems from poor alignment.
- Jaw pain or stiffness.
- Speech challenges such as lisping or unclear words.
- Noticeable tooth enamel wear.
Severe Symptoms
- Visible protrusion of the lower jaw (facial imbalance).
- Frequent tongue or cheek biting.
- Breathing issues, especially during sleep.
- Higher likelihood of TMJ disorders (jaw clicking, pain).
- Emotional stress or self-consciousness about looks.
Causes of an Underbite
Underbites rarely stem from just one reason; they usually result from genetics, habits, and growth factors. Here are the main causes:
Genetics
Genetics plays the largest role. If either parent had an underbite, their child is more likely to inherit similar jaw traits. DNA influences bone size, shape, and alignment. Common inherited features include:
- Large lower jaw (mandibular prognathism) or unusually small upper jaw.
- Uneven jaw growth rates, where the bottom jaw grows faster.
- Tooth crowding from narrow jawbones.
Childhood Habits
Early habits affect jaw growth. If they continue beyond age 3 or 4, they may cause lasting effects. Examples:
- Thumb-sucking and pacifiers: Constant sucking pushes lower teeth forward.
- Tongue-thrusting: Pressing the tongue against teeth during swallowing moves them forward.
- Mouth breathing: Ongoing nasal blockage can shift jaw position.
Injury or Trauma
Serious accidents affecting the jaw or facial bones may cause misalignment during healing. For instance:
- A broken jawbone may heal unevenly, pushing the lower jaw forward.
- TMJ damage may alter bite patterns.
Congenital Conditions
Some birth conditions affect jaw development:
- Cleft lip and palate can cause abnormal upper jaw growth, raising underbite risk.
- Disorders such as Crouzon or Treacher Collins syndromes disrupt craniofacial growth, often leading to severe skeletal underbites.
Tumours or Abnormal Growths
Though rare, tumors in the jawbone can shift growth. A growth may push one section forward or block another, creating an imbalance.
Diagnosis of an Underbite
Diagnosing an underbite involves more than just checking how the teeth look. Dentists and orthodontists use a mix of physical exams, dental imaging, and monitoring jaw growth to figure out how serious the condition is and what treatment will work best. This evaluation also helps determine whether the issue comes from dental misalignment, skeletal problems, or both.
Physical Exam
The first step is a physical exam. Here, the dentist observes how the top and bottom teeth meet when you bite down. They also check jaw movement, noting if it shifts abnormally, makes clicking sounds, or causes discomfort. Since a skeletal underbite can affect facial harmony, they also evaluate overall facial balance to see if the jaw position impacts appearance.
Dental X-rays
X-rays give a detailed look beneath the surface. They show tooth alignment, root health, and jawbone condition. These images can also reveal hidden issues such as overcrowding, extra teeth, or abnormal eruptions that may contribute to an underbite.
Cephalometric X-ray
In more complex cases, orthodontists may use a cephalometric X-ray. This type of head X-ray shows the exact relationship between the teeth, jaws, and skull. It’s especially useful when planning treatment for moderate to severe underbites, as it highlights the skeletal imbalances that need correction.
3D Imaging and Digital Scans
With modern technology, advanced tools like Cone Beam Computed Tomography (CBCT) and digital scans are now available. CBCT provides highly detailed 3D images of the jaw, which are especially helpful when planning surgery for severe skeletal underbites. Digital scans, on the other hand, allow orthodontists to design precise treatment plans for clear aligners, giving patients a more customized and comfortable option.
Child Growth Monitoring
For children, monitoring growth is a key part of diagnosis. Orthodontists track jaw development over time to spot early signs of imbalance or unusual growth. When addressed early, treatment is more effective since bones are still flexible. This can guide proper jaw development and, in many cases, reduce or even prevent the need for surgery later in life.
How to Fix Underbite
Treatment varies by age, severity, and cause. Children usually have more options since their jaws are still developing, while adults often need advanced care. After a thorough examination of your case, your dentist will suggest the best treatment for you. The options include:
- Orthodontic devices (Braces, aligners, etc.)
- Early prevention in children
- Surgery for severe cases
Orthodontic Devices for an Underbite
Braces

Traditional braces are composed of metal brackets and wires that are fixed on the surface of the teeth. They exert pressure over time to move teeth to a desirable position. They can be very effective for treating malocclusions, including an underbite.
Clear Aligners

Aligners for Teeth Straightening have emerged as a popular alternative to traditional braces. They are invisible and can be easily removed to ensure oral hygiene and routine meals.
Palatal Expanders
Palatal expanders are used to widen the top jaw in children to align it with the bottom.
Early Treatment in Children
Growth Devices
Orthodontic appliances can guide jaw growth in children, helping the upper and lower jaws align properly as they develop. Starting early often reduces the need for more invasive treatments later on.
Habit Appliances
These devices are designed to stop habits like thumb-sucking or tongue-thrusting, which can make an underbite worse. Correcting such habits early supports healthier bite development.
Regular Orthodontic Visits
Dentists recommend that children have an orthodontic evaluation by age 7. Early checkups help track jaw growth and catch problems before they become more serious.
Surgery (For Severe Adult Skeletal Underbites)
In adults, where jawbones have fully developed, surgery may be needed for severe underbites. This procedure repositions the jaws to improve both function and facial balance.
Risks if Left Untreated
Ignoring an underbite may cause long-term issues for oral health and daily life.
Dental Problems
- Tooth Wear: Misaligned bite erodes enamel, raising sensitivity and decay risk.
- Gum Disease: Harder to clean crowded teeth, increasing infection risk.
- Tooth Loss: Uneven pressure can loosen teeth.
Functional Problems
- Chewing Difficulty: A Poor bite affects digestion.
- Speech Issues: Lisping, unclear sounds, or difficulty pronouncing words.
TMJ Disorders: Jaw strain causes pain, popping, and headaches.
Aesthetic Effects
- Facial Imbalance: A Protruding jaw creates asymmetry.
- Confidence Issues: Many struggle socially or emotionally with appearance.
Breathing & Sleep Problems
- Severe underbites may contribute to sleep apnea.
- Chronic mouth breathing may also occur.
Prevention & Early Detection
While genetics can’t be avoided, good habits and early checks help reduce risks.
- Parental Role: Limit pacifier and thumb-sucking after age 3.
- Healthy Habits: Teach proper chewing and swallowing.
- Dental Visits: First orthodontic exam at age 7 (per AAO).
- Growth Checks: Regular monitoring for early detection.
Living with an Underbite
During treatment, lifestyle changes help manage symptoms.
Oral Care
- Brush twice daily and floss carefully around crowded teeth.
- Use fluoride products for added protection.
- Wear night guards if teeth grinding occurs.
Diet Tips
- Avoid sticky, hard, or chewy foods.
- Eat softer foods during orthodontic treatment.
Emotional Support
- Underbites can hurt confidence—therapy or support groups may help.
- Stay in communication with orthodontists for reassurance.
Overbite vs. Underbite
Both are malocclusions, but opposite in nature. An overbite happens when the top teeth extend far over the bottom teeth, often appearing as “buck teeth.” Mild overbites are common and usually harmless, but deep overbites can cause enamel wear, gum recession, and jaw discomfort. An underbite occurs when the bottom teeth extend beyond the top teeth, pushing the jaw forward. Overbites are generally easier to correct with orthodontics, while underbites—especially skeletal ones—may need surgery plus orthodontics. Both affect chewing, speech, and appearance if untreated, but underbites are more complex due to the bone growth links.
Fixing an Underbite
An underbite is more than a cosmetic concern; it impacts how teeth, jaws, and face work together. Though caused by genetics, habits, or trauma, today’s dentistry provides effective treatments from aligners and braces to surgery for severe cases. Detecting it early, especially in kids, makes treatment easier and prevents problems like jaw pain, speech issues, and dental damage. Adults also benefit from modern orthodontics and surgery for lasting improvement. If you see signs of an underbite in yourself or your child, visiting an orthodontist is the best next step. With timely care, you can improve both oral health and self-confidence.
FAQs
1. How do you fix an underbite?
After your dentist examines your case, they can best suggest the treatment method. For mild to moderate cases, aligners can be the ideal method. On the other hand, for severe cases, you can opt for traditional braces.
2. Is it unhealthy to have an underbite?
Yes. Untreated underbites can cause TMJ pain, dental wear, gum disease, and speech issues.
3. What’s worse, overbite or underbite?
Both have risks, but underbites are more complex to treat due to jawbone involvement.
4. What does an underbite look like?
The lower jaw and teeth extend forward, making the lower teeth more visible.
5. At what age is best to fix an underbite?
Childhood and early adolescence are ideal, but adults can still benefit from orthodontics or surgery.
6. Can I naturally fix my underbite?
Mild cases in children may improve with habit correction, but most require orthodontic treatment.
7. Do underbites get worse with age?
Yes, untreated underbites often worsen as jawbones mature.
8. What does Class III underbite look like?
A pronounced forward lower jaw with a misaligned bite.
9. What happens if you don’t fix an underbite?
Risks include jaw pain, tooth wear, gum disease, sleep apnea, and reduced confidence.
10. Does insurance cover underbite correction?
If considered medically necessary, insurance often covers part of treatment.
Citations:
Al-Mozany SA, Dalci O, Almuzian M, Gonzalez C, Tarraf NE, Ali Darendeliler M. A novel method for treatment of Class III malocclusion in growing patients (https://pubmed.ncbi.nlm.nih.gov/29226300/). Prog Orthod. 2017 Dec 11;18(1):40. Accessed 5/15/2023.
American Association of Orthodontists. 7 Common Bite Problems in Children and Adults (https://aaoinfo.org/whats-trending/7-common-bite-problems/). Accessed 5/15/2023.
Doraczynska-Kowalik A, Nelke KH, Pawlak W, Sasiadek MM, Gerber H. Genetic Factors Involved in Mandibular Prognathism (https://pubmed.ncbi.nlm.nih.gov/28570402/). J Craniofac Surg. 2017;28(5):e422-e431. Accessed 5/15/2023.
Swedish Council on Health Technology Assessment. Malocclusions and orthodontic treatment in a health perspective: a systematic review (https://pubmed.ncbi.nlm.nih.gov/28876802/). Stockholm: Swedish Council on Health Technology Assessment (SBU);2005 Oct. Accessed 5/15/2023.
